Unified clinical trial data ecosystem strategies are becoming essential as modern trials grow more complex. Protocols are more demanding, recruitment spans multiple channels, and decentralized models shift responsibilities far beyond the research site. Yet despite this evolution, many sponsors still rely on fragmented technology stacks that limit visibility, control, and operational speed.
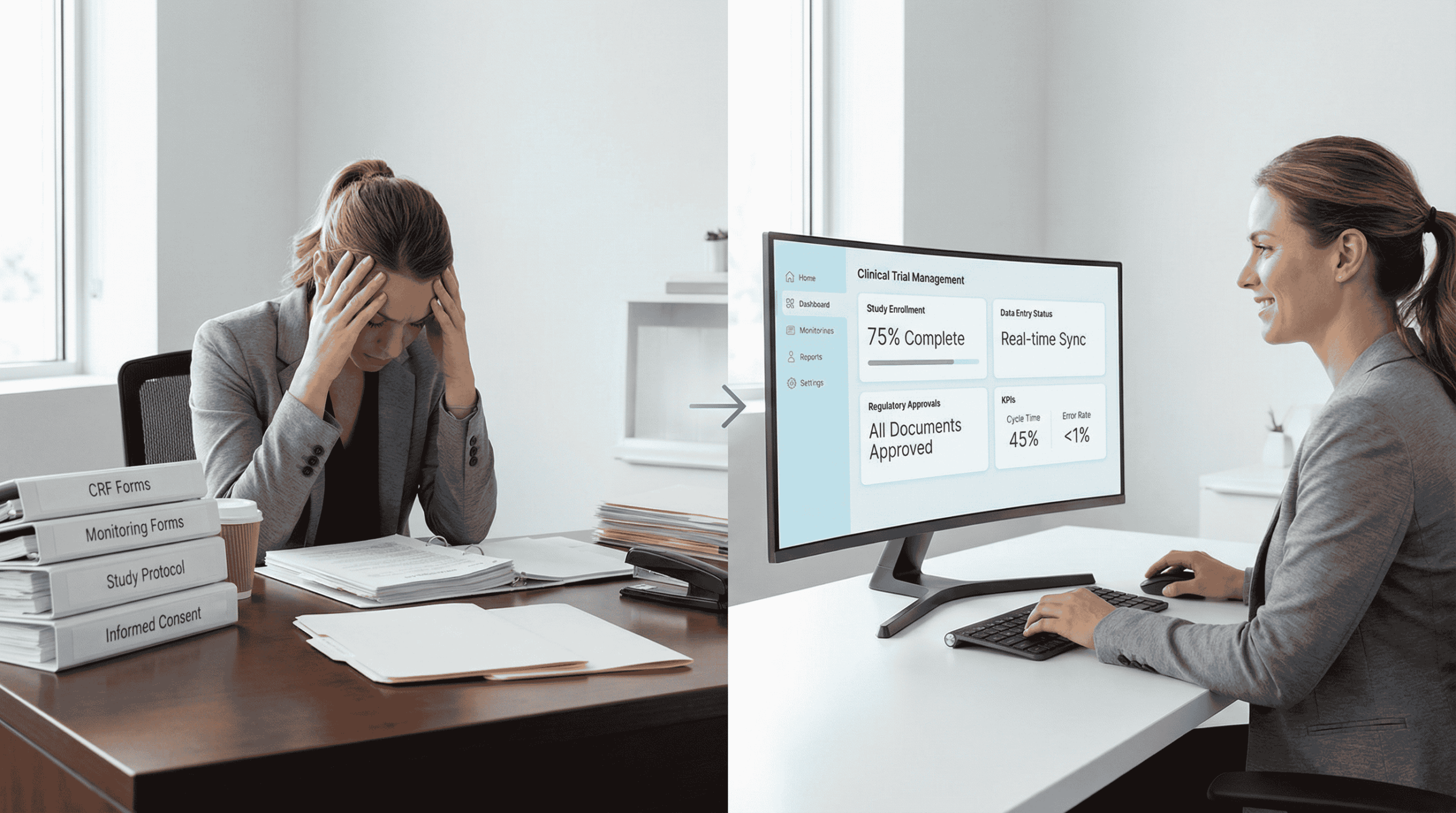
Individual platforms such as EDC (Electronic Data Capture), CTMS (Clinical Trial Management Systems), eConsent, RTSM (Randomization and Trial Supply Management), payment systems, and recruitment tools all serve important functions, but they often operate in isolation. This forces sponsors to navigate disconnected datasets, inconsistent reporting, and inefficient workflows that slow down enrollment and jeopardize trial quality.
For sponsors aiming to improve oversight, reduce timelines, and enhance data accuracy, the path forward is clear. It is time to transition from standalone tools into a unified clinical trial data ecosystem that seamlessly connects recruitment, pre-screening, site follow-up, patient interaction, and compliance workflows.
This is not simply about connecting systems. It requires true interoperability where data flows automatically, consistently, and intelligently across the entire clinical lifecycle.
The Challenge: Disconnected Clinical Systems Are Creating Operational Blind Spots
Even the most well-resourced sponsors struggle with disjointed systems. As trials expand globally, the lack of data flow between platforms like:
- Electronic Data Capture (EDC)
- Clinical Trial Management Systems (CTMS)
- Randomization and Trial Supply Management (RTSM)
- eConsent tools
- Recruitment and pre-screening systems
creates misalignment that slows decisions and increases costs.
Tufts Center for the Study of Drug Development (Tufts CSDD) reports that almost 80 percent of clinical trials experience enrollment delays, often driven by operational inefficiencies and fragmented workflows rather than a lack of patient interest.
The impact is significant.
1. Data Silos Create Delays, Errors and Slow Decisions
EDC, ePRO, CTMS, and recruitment tools rarely sync in real time. Sites frequently re-enter information across multiple systems, while sponsors must manually reconcile data to understand patient progress. This undermines the speed and accuracy needed for proactive decision-making.
2. Maintaining Multiple Systems Drives Up Costs
Each platform requires individual configuration, validation, IT support, and training. Sponsors often spend millions maintaining fragmented systems and still end up with inconsistent data.
3. Poor Site and Patient Experience Reduces Engagement
Sites may juggle several portals for scheduling, eConsent, eligibility, payments, and data entry. Patients often need separate logins for eConsent, ePRO, and communication tools. When systems are disconnected, engagement drops and retention risk increases.
4. Regulatory Compliance Becomes More Difficult
When systems are disconnected, maintaining clear documentation, consistent participant records, and dependable audit trails becomes challenging for sponsors. Data scattered across multiple tools makes it harder for teams to track actions, verify information, and stay operationally prepared. A unified ecosystem brings these elements together, offering structured workflows, cleaner documentation, and centralized visibility that strengthens overall oversight, even when individual platforms are not designed as certified regulatory systems.
Where the Real Bottleneck Begins: Recruitment, Pre-Screening and Site Follow-Up
One of the biggest pain points for sponsors is the early patient journey. Even well-funded trials struggle with:
- unclear lead-to-enrollment ratios
- dropped or untracked referrals
- duplicate pre-screening
- inconsistent communication from sites
- misaligned data about patient status
- manual handoffs between recruitment vendors, nurse teams and sites
Sponsors need a unified recruitment data clinical trials approach that connects every stage of the patient flow and provides real-time transparency into funnel performance.
This is where a unified clinical trial data ecosystem becomes transformative.
The Solution: A Unified Clinical Trial Data Ecosystem
To overcome disconnected systems, sponsors must adopt a unified ecosystem where all teams operate within a harmonized data environment. The goal is not simply integrating tools. The goal is achieving full interoperability.
Here is the difference:
| Integration | Interoperability |
| Systems connect through custom-built APIs | Systems function as one ecosystem by design |
| Requires manual reconciliation | Eliminates manual reconciliation |
| Data flow delays are common | Data flows instantly across all platforms |
| High IT maintenance | Minimal IT oversight |
| Inconsistent data formats | Standardized data structures |
True interoperability links recruitment, screening, site activity, data capture, monitoring, and compliance into one cohesive operational engine.
How a Unified Clinical Trial Data Ecosystem Works for Sponsors
Below is how a modern unified ecosystem improves operational clarity and speed for sponsors.
1. Seamless Recruitment and Pre-Screening Integration
Participants enter through digital recruitment channels and their data automatically flows into a centralized platform. Nurse teams conduct pre-screening and eligibility reviews in the same environment. Sponsors gain real-time visibility across:
- lead conversion
- channel performance
- drop-off stages
- referral timing
- qualification metrics
This supports more accurate forecasting and spend optimization.
2. Real-Time Site Follow-Up and Visit Tracking
Sites receive referrals in a structured dashboard rather than email threads. Every action such as phone attempts, scheduling, prescreen outcomes, and screen fail reasons is visible to sponsors instantly. This removes site communication gaps and improves clinical trial performance improvement.
3. Fully Connected EDC, CTMS and RTSM
Instead of entering the same information into multiple systems, a unified ecosystem ensures that:
- EDC receives verified, qualified participants
- CTMS updates trial milestones automatically
- RTSM aligns with actual site visit schedules
This reduces drug waste, protocol deviations, and manual reconciliation.
4. Unified Compliance and Centralized Audit Trails
With a connected workflow, sponsors gain clearer documentation, structured participant records, and centralized communication logs that make oversight easier. All actions related to pre-screening, referral, and site follow-up are captured in one place, reducing manual tracking and helping study teams maintain better operational visibility. This improves monitoring efficiency, supports inspection readiness from an operational standpoint, and reduces the risk of missing critical information during study execution.
5. A Single User Interface for Sites and Patients
Instead of accessing multiple portals, sites and patients use one platform for consent, ePRO, scheduling, payments, and communication. Research shows that a simplified digital experience can increase patient retention by 25 to 40 percent. This improvement directly benefits sponsor timelines and reduces trial dropouts.
The DecenTrialz Advantage: A Unified Recruitment and Screening Ecosystem for Modern Sponsors
DecenTrialz was developed to eliminate fragmentation and give sponsors a complete operational view from first participant contact to enrollment. The platform unifies:
A Structured Pre-Screening Process From Start to Referral
- Study requirements are organized into a clear framework
- Participants review and complete eConsent
- Participants answer guided pre-screening questions
- A Registered Nurse follows up and asks study-related questions
- Qualified participants are referred to the site
Sponsors gain:
Real-time visibility: Instant insights without chasing weekly reports.
Operational efficiency: Reduced manual work and fewer errors.
Faster enrollment timelines: Because every step of the funnel works together.
Lower operational costs: No more system sprawl or expensive integrations.
High-quality clinical trial data: Supporting confident and accurate decision-making.
The Future of Clinical Trials Depends on Unified and Connected Data
Sponsors can no longer rely on fragmented tools if they want to accelerate timelines, improve trial quality, and operate with confidence. The future of clinical research lies in unified clinical trial data ecosystems that connect recruitment, screening, site operations, EDC, CTMS, RTSM, and compliance into one seamless workflow.
Unified environments support:
- consistent and accurate data
- faster decision-making
- improved site and patient experiences
- better compliance
- higher enrollment performance
It is time for sponsors to move beyond disconnected systems and adopt a unified, interoperable ecosystem that brings clarity and control back to clinical operations.