In the world of clinical trials, ensuring compliance, data integrity, and patient safety through regular site audits has always been a fundamental aspect of maintaining trial quality. However, the landscape is changing. The global shift toward remote and decentralized trial models accelerated by the pandemic, has dramatically transformed how CROs (Contract Research Organizations) manage site oversight. Virtual audits are no longer just a temporary solution; they are becoming a permanent and necessary part of clinical trial operations.
This shift is more than a logistical adjustment; it’s a strategic evolution that can help CROs enhance trial efficiency and reduce costs, all while ensuring compliance and safety. Let’s explore how CROs are embracing virtual site audits, the tools that are enabling this transformation, and why this approach is here to stay.
Why Audits Matter in Clinical Trials
Ensuring Compliance, Data Integrity, and Patient Safety
The integrity of a clinical trial depends on rigorous audits. These audits ensure compliance with regulatory standards, protect patient safety, and guarantee that data collected during trials is accurate and trustworthy. Any lapse in these areas can lead to regulatory penalties, compromised patient safety, and, ultimately, unreliable trial results.
For CROs, maintaining the highest standards of oversight is non-negotiable. These audits not only safeguard public trust in clinical research but also protect sponsors’ investments and help ensure that a trial can proceed smoothly from start to finish.
The CRO’s Role in Maintaining Standards
CROs play a pivotal role in managing trial operations. Ensuring that clinical trials adhere to regulatory requirements such as GCP (Good Clinical Practice), ICH-GCP (International Council for Harmonisation of Good Clinical Practice), and FDA standards is essential. With the growing complexity of clinical trials, it’s no longer enough to rely on periodic onsite visits to ensure compliance, CROs must implement systems that allow for continuous oversight, even when physical site visits are not possible.
The Shift to Virtual Audits: A Response to Changing Needs
The pandemic has fundamentally altered how clinical trials are conducted. Travel restrictions and health protocols led many CROs to adopt virtual-first approaches to trial management, including remote site audits. What started as a necessity during COVID-19 has quickly evolved into a model that offers several advantages over traditional onsite audits.
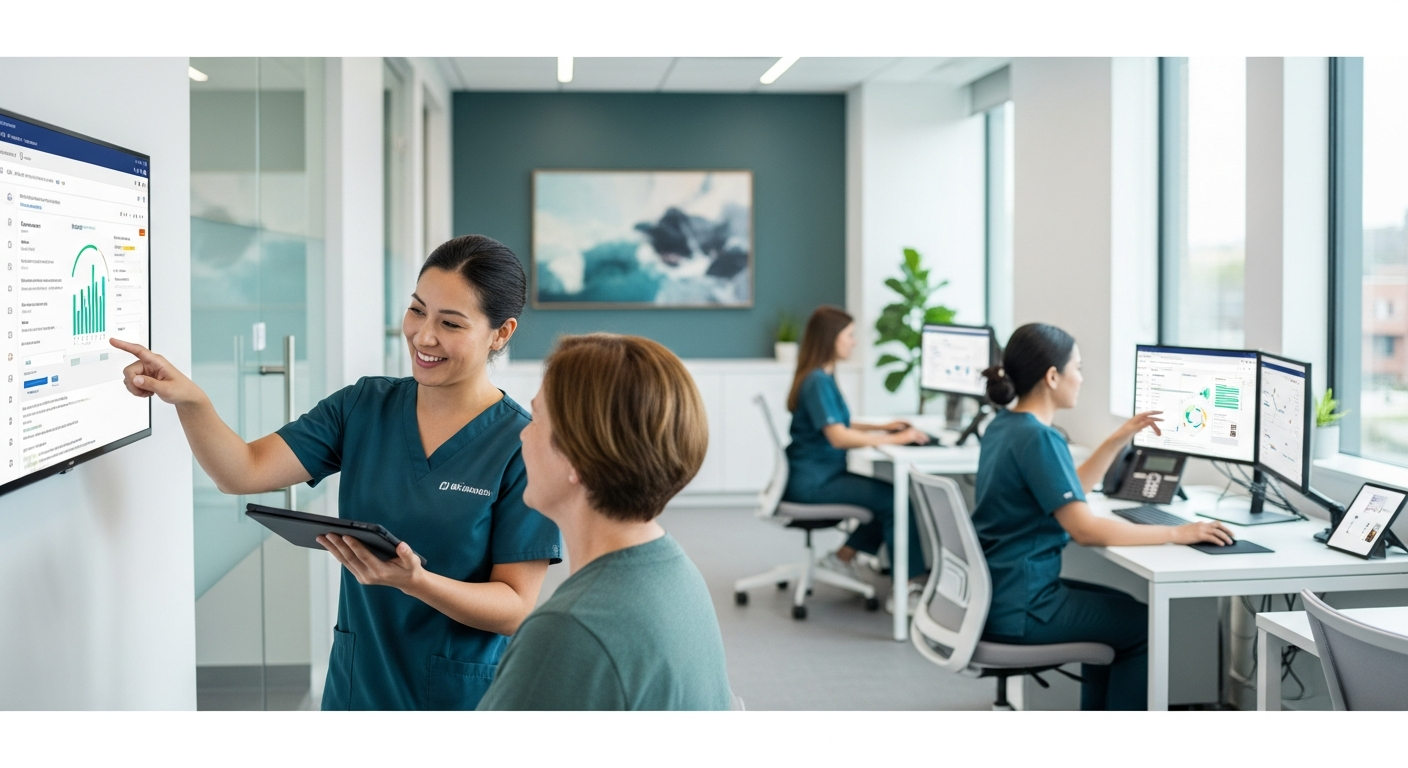
How Virtual Audits Benefit CROs and Sites
Virtual audits remove the logistical challenges of traveling to and from trial sites, cutting down costs and allowing for more flexible scheduling. They also offer sites the opportunity to engage with auditors without the disruption of hosting an onsite visit. This shift allows CROs to conduct audits in parallel across multiple sites, speeding up oversight and making it easier to identify potential issues before they become major problems.
For sites, virtual audits reduce the burden of preparing for and accommodating auditors on-site. Additionally, they provide more flexibility for site staff to continue their regular duties without the interruption of an onsite audit, making them more efficient overall.
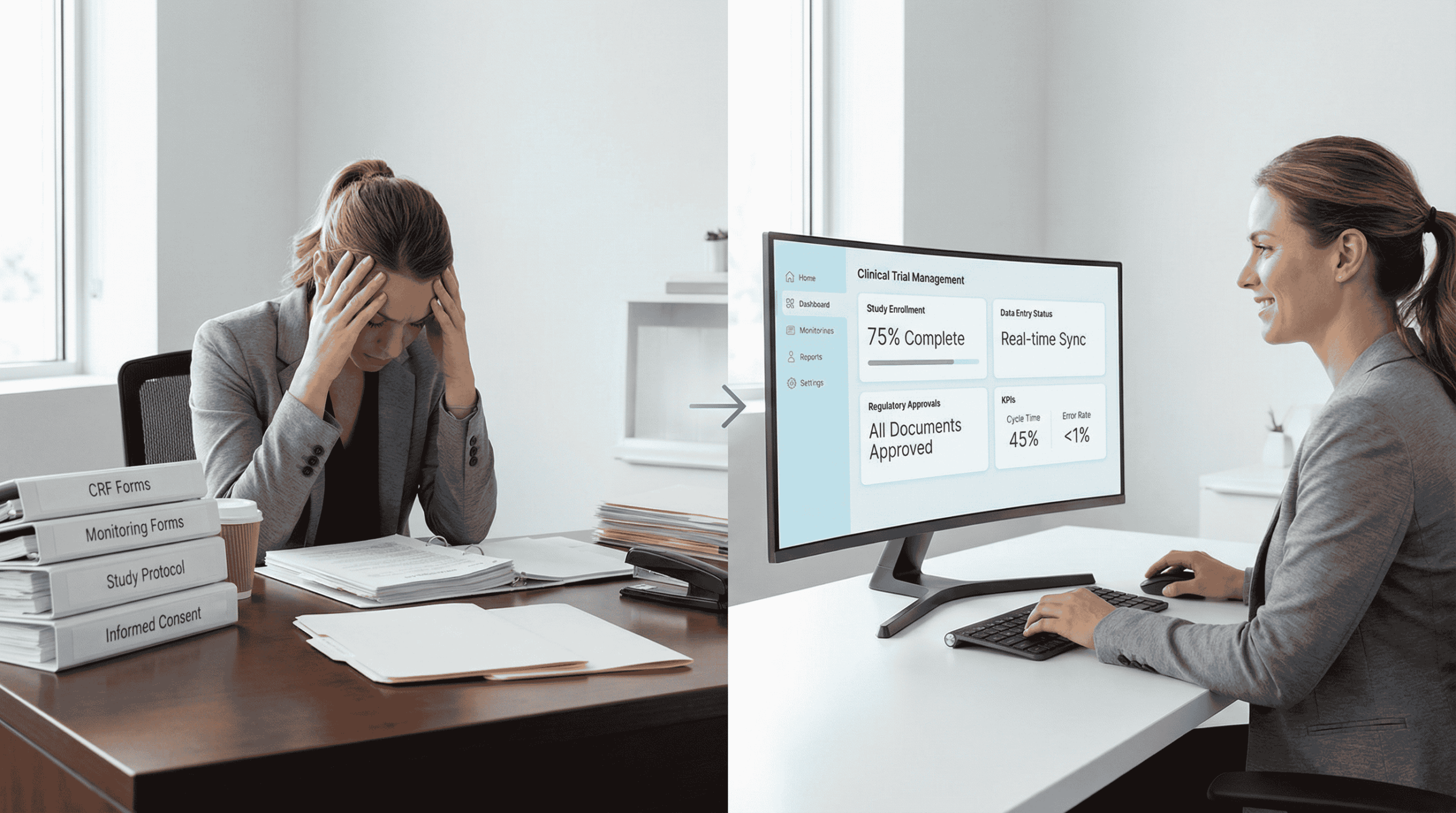
Tools & Technologies Enabling Virtual Site Monitoring
For virtual site audits to be effective, CROs need the right tools and technologies. The integration of secure, cloud-based platforms, real-time dashboards, and monitoring tools has made remote audits not only possible but efficient and reliable.
Real-Time Monitoring Dashboards
DecenTrialz provides a Real-Time Dashboard that delivers live updates on the status of clinical trials, ensuring transparency and efficiency for all stakeholders. Through this platform, Sponsors, CROs, and research sites can track participant enrollment, confirm patient eligibility, and monitor trial progress in real time.
Cloud-Based Document Management
Cloud platforms facilitate easy document sharing and storage, allowing auditors and site staff to access trial-related materials at any time, from anywhere. These platforms ensure that data is securely stored and easily accessible, which improves transparency and supports better decision-making during virtual audits.
AI and Automation
Artificial intelligence (AI) is also playing a key role in virtual site audits. By automating data analysis and identifying potential compliance risks, AI tools help auditors prioritize issues that need attention, saving time and improving the accuracy of audits. These tools also provide predictive insights, helping CROs spot trends that may indicate emerging risks, allowing for proactive management.
Ensuring Compliance in Remote Audits: Best Practices for CROs
While virtual audits offer numerous advantages, they also require careful management to ensure compliance and maintain data security. Here are some best practices that CROs should adopt to maximize the effectiveness of remote audits:
Maintaining Transparency with Regulators
Clear communication with regulatory authorities is crucial in virtual audits. CROs should ensure that all audit processes are thoroughly documented and that communications with sites are transparent. Secure digital platforms can provide an audit trail, which makes it easier to share information with regulators and ensures that the entire audit process is verifiable and compliant.
Data Security and Handling
Security is paramount when conducting remote audits. CROs should ensure that platforms used for audits comply with data protection regulations such as HIPAA, ISO and GDPR. These platforms should provide encryption, secure data storage, and controlled access to ensure the privacy and security of sensitive trial data.
Clear Communication and Documentation
Good communication is essential for a successful virtual audit. CROs should establish protocols for how audits will be conducted, how documentation will be shared, and how results will be communicated. This ensures that everyone involved knows their responsibilities and that the audit process runs smoothly.
Monitoring Patient Safety in Real-Time
Real-time monitoring tools should be used to track patient safety metrics, recruitment progress, and data collection, ensuring that everything is on track and compliant with regulatory standards. These tools help to quickly identify any discrepancies or safety concerns, enabling CROs to act immediately, even in a virtual environment.
Virtual Audits Are Here to Stay
The shift to virtual audits represents a major change in how CROs conduct trial oversight. This transformation isn’t just a temporary measure, it’s a permanent shift that offers greater efficiency, improved compliance, and reduced costs for all parties involved. As the clinical trial industry continues to embrace remote and decentralized trial models, virtual audits will remain a critical component of ensuring trial integrity.
The Future of Remote Audits
Looking ahead, we can expect the use of AI, machine learning, and automation in remote audits to become more widespread. These technologies will further streamline the audit process, improve efficiency, and enhance the accuracy of monitoring, allowing CROs to conduct audits faster and more effectively. Additionally, hybrid models that combine in-person and virtual audits will likely become more common, offering flexibility and ensuring the best approach for each trial.