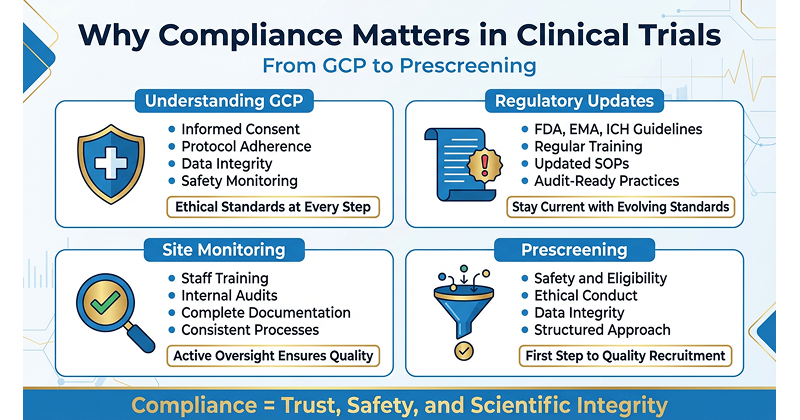
Compliance is the backbone of ethical and successful clinical trials. Every research site needs to follow compliance standards to protect participants and produce trustworthy results. When guidelines are followed step by step, participants remain safe, data stays reliable, and the site earns trust. On the flip side, faults in compliance can put patients at risk, damage data quality, and harm a site’s reputation.
Understanding Good Clinical Practice (GCP)
At the center of compliance in clinical trials are Good Clinical Practice (GCP) guidelines. These international ethical and scientific standards set the rules for designing, conducting, recording, and reporting clinical studies. They show how a trial should be managed to safeguard participants and ensure reliable data.
Key principles of GCP include:
Informed Consent: Participants must willingly agree to join after understanding the purpose, process, risks, and potential benefits of the trial.
Protocol Adherence: Stick to the trial protocol without making unauthorized changes. The protocol is the study’s blueprint, and following it ensures scientific integrity.
Data Integrity: Data must be recorded accurately and fully. Each observation and outcome needs to be documented so findings are dependable and verifiable.
Safety Monitoring: Watch participant health carefully and report adverse events quickly to identify risks early and respond promptly.
Regulators worldwide expect strict GCP compliance, but more importantly, it’s about doing right by the participants.
Staying Up-to-Date with Regulations
Clinical trial regulations are constantly evolving. As science advances and new challenges surface, requirements shift. Research sites must stay alert and adapt to keep up.
This involves tracking updates from authorities such as the FDA, EMA, ICH, and local regulators, then adjusting practices accordingly. New requirements may affect privacy, data handling, or reporting standards. To stay compliant, sites should review bulletins regularly, attend workshops, and update their Standard Operating Procedures (SOPs) and training materials when needed. Keeping pace with regulations ensures sites remain aligned with current expectations.
Site-Level Compliance Monitoring
Even with solid plans, everyday operations require oversight. Site-level monitoring means catching and correcting problems before they escalate.
Training & Procedures: Staff must be well-trained in GCP, the trial protocol, and site SOPs. Ongoing refreshers keep them current.
Internal Audits: Conduct periodic audits of records and processes. For instance, check that consent forms are properly signed and that data entries match source documents. These checks identify issues like missing records or protocol deviations early.
Thorough Documentation: Ensure trial records are complete and updated. If it isn’t documented, it didn’t happen.
By monitoring closely, sites create a culture of quality and preparedness. External audits then become smoother, with fewer surprises. Most importantly, it safeguards participants and protects the credibility of the research.
The Importance of Ethical Standards
Ethics drive clinical research, and compliance is how those ethics come alive in practice. Areas like participant protection, informed consent, and transparency highlight the connection between the two.
Participant Protection: Trials must prioritize the rights and well-being of participants. Continuous monitoring and ethics board oversight help reduce risks, and if serious concerns arise, ethical sites act immediately.
Informed Consent: Beyond being a legal requirement, informed consent is an ethical obligation. Using approved forms and plain language helps participants truly understand the study. They should know their participation is voluntary and that they can withdraw at any time.
Data Transparency: Honesty is crucial in research. Compliance means reporting results truthfully, avoiding data manipulation, and following requirements to register and publish trial outcomes. This openness builds trust with the public.
Adhering to ethical principles through compliance ensures participant protection and data credibility, while also maintaining public confidence in clinical trials.
Pre-screening Compliance
Prescreening is the first step in identifying potential participants, usually by checking basic eligibility criteria before enrollment. Done correctly, it speeds up recruitment, but it must remain accurate and ethical.
Why compliance matters in prescreening:
Safety and Eligibility: Only participants who meet the criteria should proceed. This protects individuals from unsafe interventions.
Ethical Conduct: Since prescreening happens before formal consent, sites must use IRB-approved scripts, collect only necessary data, and ensure participants know this step is voluntary and confidential.
Data Integrity: Accurate prescreening prevents the wrong candidates from enrolling, avoiding protocol violations and unreliable results.
Platforms like DecenTrialz help sites manage this prescreening process while staying aligned with GCP and compliance requirements. This reduces rejections later, ensures only eligible volunteers advance, and makes trial operations smoother and more efficient.
From GCP to prescreening, compliance runs through every layer of a clinical trial. It’s not about ticking boxes,it’s about protecting participants and maintaining the quality of science.
For research sites, strong compliance means credibility. Regulators and sponsors recognize high standards, and participants are more likely to trust ethical sites. Ultimately, compliance forms the foundation for every responsible trial, allowing new treatments to be tested safely while earning and keeping public trust.
Leave a Reply