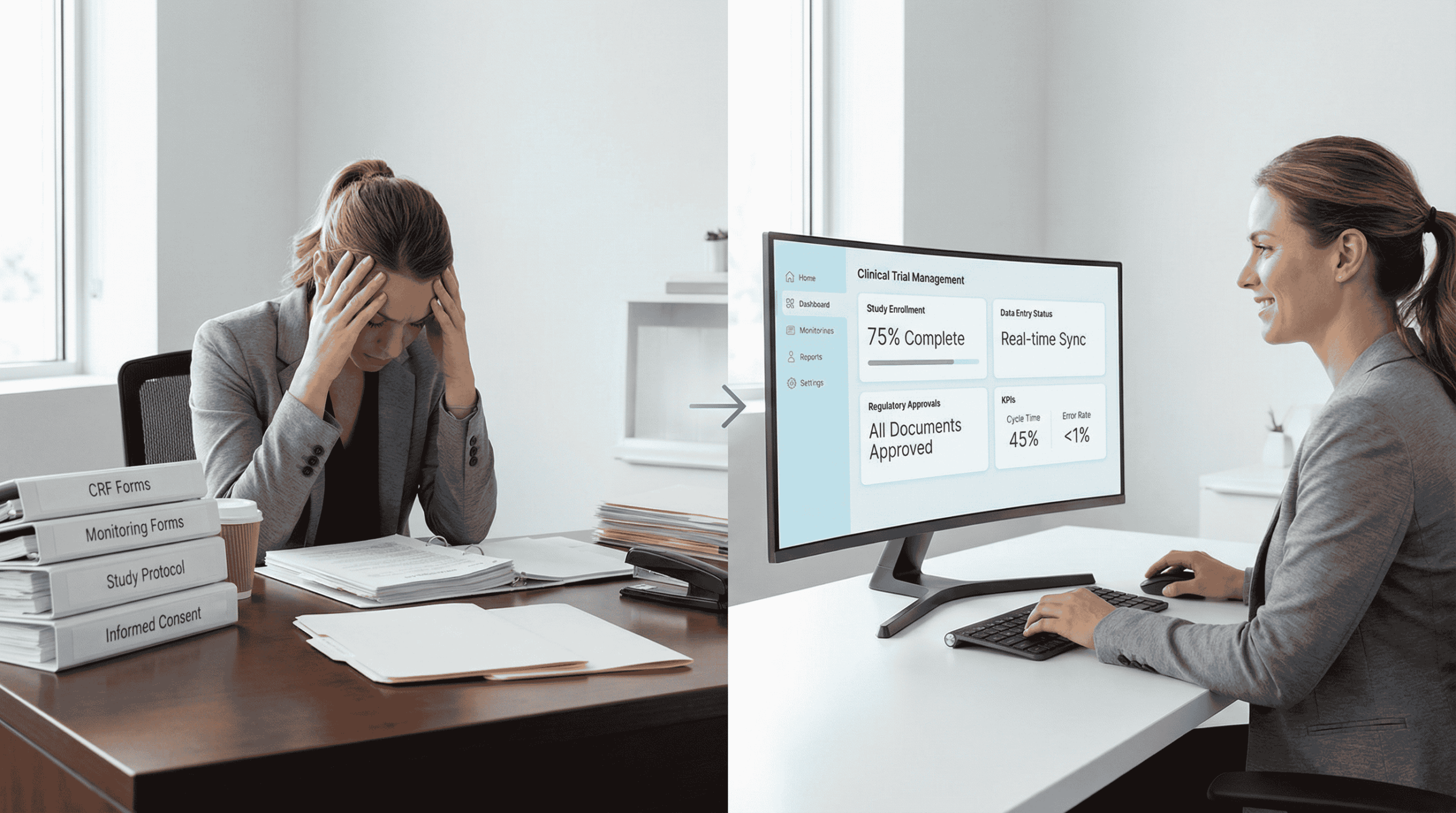
Running a clinical trial at the site level is as much about managing people and processes as it is about advancing science. Research coordinators, investigators, and support staff often carry a heavy load that goes far beyond participant care. Between regulatory paperwork, recruitment tracking, and sponsor reporting, site staff can feel buried in administrative demands.
That is why improving site efficiency clinical trials has become one of the most important priorities in modern research. Reducing administrative burden is not just about saving time; it directly impacts enrollment speed, data accuracy, staff satisfaction, and ultimately, trial success.
The Reality of Site Burdens
Clinical trial sites are often stretched thin. A single coordinator may be juggling multiple studies, each with unique requirements, reporting systems, and sponsor expectations. Some of the most common site burdens include:
- Complex regulatory paperwork that requires constant updates and detailed records.
- Manual data entry across multiple platforms, increasing the chance of errors.
- Recruitment tracking that demands hours of screening candidates who may not qualify.
- Communication gaps between sites and sponsors that cause delays or duplicated work.
These challenges do not just slow trials down. They contribute to staff burnout, high turnover rates, and frustration among site teams who want to focus on participant experience and quality of care.
Workflow Optimization: Smarter, Not Harder
One of the most effective ways to achieve site burden reduction is through smarter workflows. Instead of simply adding more staff to carry the workload, sites can rethink how everyday processes are handled.
Key strategies for workflow optimization include:
- Standardizing procedures: Developing templates for documentation, consent, and reporting to reduce variation.
- Centralizing information: Storing data in one system rather than juggling multiple platforms.
- Automating repetitive tasks: Using digital tools to manage scheduling reminders, eligibility pre-screening, and routine follow-ups.
- Delegating effectively: Ensuring that tasks are assigned to the right team member, whether administrative or clinical.
By streamlining these steps, research sites can focus more of their time on direct participant engagement instead of paperwork.
Communication Between Sponsors and Sites
Strong communication between sponsors and research sites is essential for reducing administrative workload. Too often, sites are left with unclear instructions, overlapping data requests, or delayed feedback from sponsors. This results in unnecessary duplication and wasted time.
Improved sponsor–site communication can deliver major benefits:
- Faster resolution of protocol questions.
- Clearer expectations for reporting timelines.
- Reduced redundancy in monitoring and documentation.
- Stronger alignment on recruitment and retention strategies.
When sponsors treat sites as true partners, administrative stress is reduced and trial performance improves.
Technology as a Partner for Efficiency
Technology plays an increasingly important role in workflow automation and research site management. The right tools can minimize manual work while ensuring compliance and data quality.
Examples include:
- Electronic Trial Master Files (eTMF): Streamlined document storage and version tracking.
- Electronic Data Capture (EDC) systems: Real-time data entry with built-in validation.
- Pre-screening platforms: Automatically filter out ineligible candidates.
- Participant engagement tools: Send automated reminders for visits and medication adherence.
With DecenTrialz filtering out ineligible candidates, sites can save hours of manual pre-screening and focus their administrative time on participants who are more likely to enroll. This not only improves efficiency but also boosts staff morale by reducing repetitive tasks.
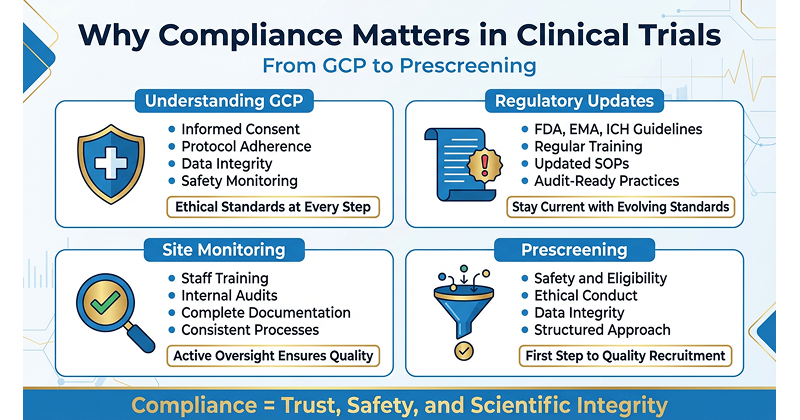
Balancing Compliance and Efficiency
A common concern for sites is that cutting down administrative work may lead to compliance risks. The key is not to eliminate necessary processes but to make them easier to manage.
- Automated systems ensure audit trails are maintained.
- Standardized templates reduce the risk of missing critical information.
- Digital communication tools allow for faster reporting to sponsors and regulators.
In this way, sites can maintain compliance while also improving day-to-day efficiency.
The Human Impact of Reduced Burden
When administrative load is reduced, the benefits ripple across the entire trial process. Site staff experience less stress and burnout, retention improves, and participants receive more focused attention. Ultimately, smoother workflows mean trials progress faster and with fewer errors.
Research site management is not just about paperwork. It is about creating an environment where skilled professionals can use their expertise effectively. By prioritizing efficiency, sites can transform from being overwhelmed by tasks to being empowered to deliver higher-quality research.
Technology as a Partner in Site Efficiency
Another important piece of site efficiency in clinical trials is how technology supports the day-to-day work of coordinators and investigators. Tools that automate scheduling, reduce duplicate data entry, and centralize communication channels can cut down on hours of repetitive work each week. When sites spend less time wrestling with paperwork or manual tracking, they have more time to focus on participants and protocol accuracy. This balance not only improves staff satisfaction but also ensures that trial outcomes are measured with greater precision. As the industry moves forward, technology will continue to play a central role in combining efficiency with quality.
Moving Forward
The future of clinical trials depends on strong, efficient sites that can balance regulatory demands with participant care. Sponsors, regulators, and technology providers all play a role in supporting this shift.
By embracing workflow automation, enhancing sponsor–site communication, and adopting platforms like DecenTrialz, research sites can reduce their administrative burden while staying compliant and participant-focused.
Improving site efficiency clinical trials is not just an operational goal. It is a step toward building a sustainable research environment where both staff and participants feel supported, and where breakthroughs can reach healthcare faster.