Recruitment is one of the toughest challenges in clinical research. Many trials face delays or even risk closing early because not enough participants can be enrolled on time. Sponsors often invest heavily in outreach campaigns, yet one of the most effective channels is often overlooked: community physicians.
These are the doctors patients already know and trust, such as family doctors, specialists, or local clinic providers. By engaging these physicians in the referral process, sponsors and research sites can connect with potential participants sooner, build trust faster, and avoid the common roadblocks that slow down recruitment.
This article looks at why partnering with local physicians matters, how to make those partnerships work, and the safeguards needed to keep referrals ethical and efficient.
The Role of Community Physicians in Clinical Trial Recruitment
Community physicians are in a unique position when it comes to clinical trial referrals. Unlike advertisements or online listings, a recommendation from a trusted doctor carries weight. Patients are more open to listening because the information comes from someone who already understands their health history and personal circumstances.
These physicians can explain trial opportunities in plain language, answer questions on the spot, and help patients make informed choices. They are also better able to clear up misconceptions and highlight the potential benefits of participation.
For these reasons, engaging local doctors is one of the most reliable ways to grow participant pools and improve trial diversity.
Myth: Physicians Are Too Busy or Uninterested in Clinical Trials
It is often assumed that physicians do not have the time or interest to refer patients to trials. The reality is different. Most doctors are supportive of research but face real barriers, such as:
- Not knowing about available trials
- Complicated eligibility criteria
- Referral processes that take too much time
These hurdles can be solved. Short trial summaries, clear checklists, and easy referral forms make it much more realistic for physicians to participate. When the process is simple and transparent, doctors are far more willing to get involved.
Benefits of Partnering with Community Physicians
1. Broader and more diverse reach
Doctors serve patients across all walks of life, including rural areas and underrepresented groups. Their involvement helps sponsors meet diversity goals that regulators are increasingly prioritizing.
2. Higher trust and enrollment rates
When a physician introduces a trial, patients are more likely to consider it seriously. That trust speeds up decision-making and often leads to higher enrollment rates.
3. Sustainable referral networks
Strong sponsor–physician relationships do not just help with one study. They create a long-term pipeline for future trials.
Example: In one oncology program, collaboration with a regional network of primary care physicians helped the sponsor shorten the time to first-patient enrollment compared to prior site-only recruitment approaches.
Best Practices for Engaging Physicians
- Keep information short and clear: Provide one-page trial summaries with eligibility details, patient commitment, and key benefits.
- Offer educational resources: Short webinars, lunch-and-learn sessions, or quick guides help physicians feel comfortable presenting trial options.
- Stay responsive: Assign a liaison who can quickly answer physician questions. Consistent support builds trust and encourages repeat referrals.
Creating a Smooth Referral Process
Digital trial-matching tools
With patient consent, digital trial-matching tools allow physicians to enter a small set of relevant details and quickly identify potential study options. By using AI-powered trial matching, these tools help align patient profiles with study eligibility criteria while reducing manual effort for busy clinical practices.
Such approaches help minimize administrative burden and make it easier for physicians to participate in research referrals without disrupting routine care.
How DecenTrialz supports physician referrals
DecenTrialz supports physician participation by offering structured digital pre-screeners and secure referral workflows that simplify how patient information is reviewed and shared with research sites. This approach helps physicians remain engaged in the referral process while allowing research teams to manage follow-up efficiently and responsibly.
Building Awareness in the Community
- Co-host local events: Health fairs, screenings, or seminars with community doctors can raise awareness.
- Share patient stories: With permission, highlight positive trial experiences in newsletters or clinic waiting rooms.
- Use local media: Joint interviews or articles with trusted physicians build credibility.
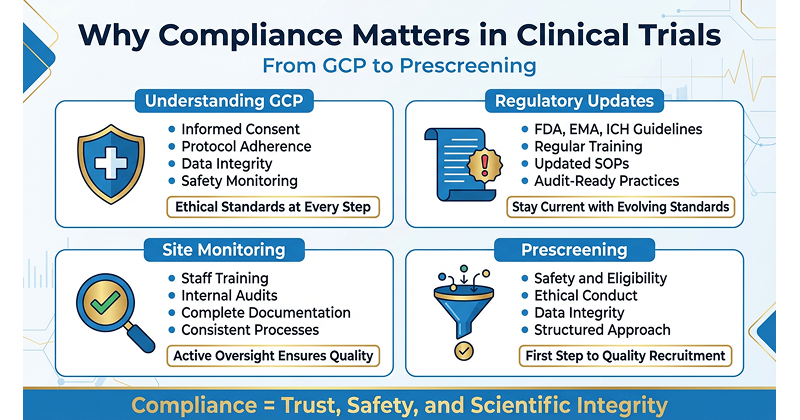
Compliance and Ethical Safeguards
Physician referrals must always be handled with care:
- Patient privacy: Every referral must comply with HIPAA and local data protection laws. Patient consent is essential before sharing information.
- Transparency in incentives: Any support provided to physicians should be appropriate, clearly disclosed, and aligned with applicable regulations and ethical guidelines.
- IRB oversight: Referral processes and consent language should always go through IRB or ethics committee review.
- Secure communication: Use encrypted systems, not personal email or fax, for any data transfer.
Key Note: Physician engagement only works if it is transparent, compliant, and ethical. Trust is the foundation of every referral.
The Role of DecenTrialz
DecenTrialz does not run trials, but it provides the secure infrastructure that makes physician involvement easier. The platform includes:
- Digital pre-screeners to confirm eligibility upfront
- Automated trial-matching tools
- Referral tracking dashboards for transparency
Physicians and research teams can explore ongoing study opportunities through DecenTrialz, helping align patients with trials that may be relevant to their care journey.
This reduces the workload for doctors, shortens recruitment timelines, and strengthens sponsor–physician collaboration.
Conclusion
Community physicians are a powerful yet underused resource in clinical trial recruitment. Their trust, local knowledge, and access to diverse patient populations can make the difference between a delayed study and a successful one.
By addressing misconceptions, simplifying referral processes, and maintaining strict compliance safeguards, sponsors can build strong partnerships that last beyond a single trial.
Platforms like DecenTrialz help make these connections practical, secure, and sustainable. The result is faster recruitment, more representative trials, and stronger trust between patients, providers, and the research community.