In clinical research, data is everything. It is not just numbers on a spreadsheet. It represents the safety of participants, the credibility of results, and whether a treatment is ultimately approved. Without accurate, reliable data, even the most promising study can lose momentum.
At the site level, where data is first collected, clinical data management (CDM) determines whether a trial succeeds or fails. Every patient history, lab result, and entry into an electronic case report form (eCRF) must be captured, verified, and stored with precision. When site teams get this right, every decision later in the trial, from safety reviews to final analysis, is built on trustworthy evidence. For an overview of how trial operations connect together, see our guide on Clinical Trial Management Systems: The Backbone of Site Operations.
What is Clinical Data Management?
Clinical data management (CDM) is the process of collecting, cleaning, and safeguarding trial data so that it is accurate, complete, and compliant. It begins with the first data entry at a site and continues until the database is locked for analysis.
In simple terms, effective CDM means:
- Data is correct, with no errors or unexplained gaps.
- Information is consistent across all sources.
- Sensitive details are protected under HIPAA and related privacy rules.
Without strong site-level CDM, the integrity of the entire trial is at risk.
Why Site-Level Data Management Matters
The trial site is the first point where data enters the system. That makes it the most important checkpoint for accuracy. If errors happen here, they spread through the study.
Strong site-level CDM matters because:
- First capture is critical: It is easier to prevent mistakes early than to fix them later.
- It avoids delays: Clean data reduces the need for repeated checks during monitoring.
- It improves quality: Reliable site data strengthens the statistical value of trial results.
- It reduces deviations: Accurate entries lower the risk of protocol violations.
- It helps oversight: Real-time, accurate data supports sponsor and CRO monitoring.
When sites prioritize accuracy at the source, they reduce costly rework and keep studies on schedule.
Ensuring Data Integrity
Regulatory agencies such as the FDA and EMA set clear expectations for data. Clinical trial data must be:
- Accurate: It must reflect the true measurement or observation.
- Complete: No missing values should remain without explanation.
- Traceable: Every change must leave a record of who made it, when, and why.
To meet these standards, sites rely on practices such as:
- Source Data Verification (SDV): Comparing database entries with original medical records.
- Audit trails: Recording every edit to maintain transparency.
- 21 CFR Part 11 compliance: Ensuring electronic records and signatures are secure and valid.
These steps, aligned with ICH-GCP standards, safeguard both data quality and patient safety.
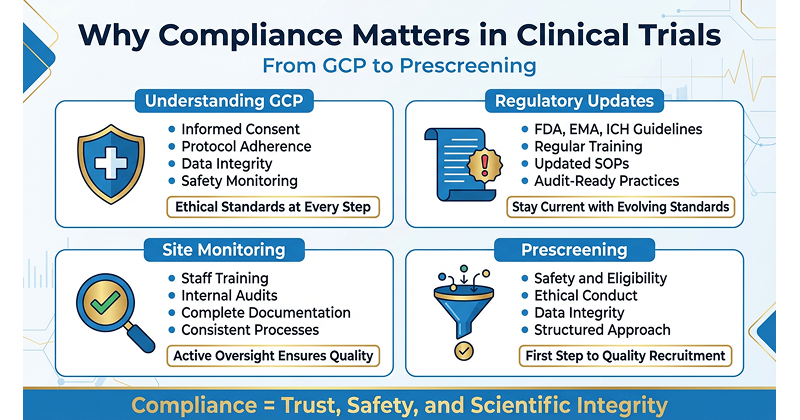
Compliance and Audit Readiness
Good data management is more than a best practice. It is a regulatory requirement.
- ICH-GCP: Ensures data is credible and reported according to protocol.
- HIPAA: Protects participant privacy and health information.
- Audit preparedness: Sites must be ready for inspections at any time. Missing or inconsistent records can quickly lead to findings.
When compliance is part of daily site workflows, audits become less stressful and more predictable.
The Role of a Clinical Trial Management System (CTMS)
Technology is a powerful tool for improving data management. A Clinical Trial Management System (CTMS) helps sites manage trial operations and supports better data quality.
The benefits of a CTMS include:
- Centralized, secure storage of all records.
- Automated tracking for visits, labs, and data queries.
- Query resolution tools for faster responses to monitors.
When paired with an Electronic Data Capture (EDC) system, a CTMS creates seamless workflows that reduce errors and improve efficiency. This connection between operations and data integrity is one reason we emphasize CTMS in our blog on How CROs Power Every Phase of Clinical Trials.
Best Practices for Site-Level Data Management
Sites that consistently produce high-quality data usually follow a few proven practices:
- Follow SOPs: Always work according to Standard Operating Procedures.
- Enter data promptly: Capture information as soon as possible to avoid mistakes.
- Verify source data: Regularly compare eCRFs with original documents.
- Use consistent formats: Standardize units, dates, and terminology across the team.
- Invest in training: Provide regular staff training on EDC systems and SOPs.
- Resolve queries quickly: Address sponsor and monitor queries without delay.
Common Pitfalls to Avoid
Even experienced sites can run into problems if they do not watch for these issues:
- Delayed entries: Waiting too long increases the chance of errors.
- Incomplete documentation: Missing signatures, dates, or lab values cause compliance gaps.
- Inconsistent reporting: Using different formats for similar data points leads to confusion.
- Overuse of paper: Failing to move records into digital systems on time creates risks.
Avoiding these pitfalls makes site operations smoother and strengthens trust with sponsors.
Conclusion
Site-level clinical data management is not just a technical step. It is the backbone of trial integrity, participant safety, and regulatory compliance. By focusing on accurate, timely, and compliant data practices, sites protect patients, improve study outcomes, and maintain credibility with sponsors.
With the right systems, such as CTMS and EDC tools, sites can reduce delays, ensure audit readiness, and contribute to reliable scientific discovery. Strong CDM keeps trials moving forward and ensures that the evidence behind new treatments is solid.