Joining a clinical trial can feel unfamiliar at first, especially if you have never participated in research before. Many people feel uncertain about what will happen, how long the process takes, or whether it is safe.
This uncertainty is normal. The good news is that joining a clinical trial follows a clear, structured, and transparent process designed to protect participants at every stage. You are always informed, supported, and free to make choices that feel right for you.
This guide walks you through the entire journey in simple, reassuring language so you know exactly what to expect.
For many people, joining a clinical trial is their first interaction with medical research, which is why clarity and transparency matter.
What Does Joining a Clinical Trial Mean?
Joining a clinical trial means choosing to take part in medical research that helps doctors and researchers learn more about treatments, medications, or ways to improve care.
Clinical trials are carefully regulated and always voluntary. Participants are never required to continue if they feel uncomfortable, and safety is monitored throughout the study. You are given clear information before making any decisions and can ask questions at any time. There is no obligation to participate, and choosing not to join does not affect your regular medical care.
Understanding what joining a clinical trial involves helps participants feel confident and informed before deciding.
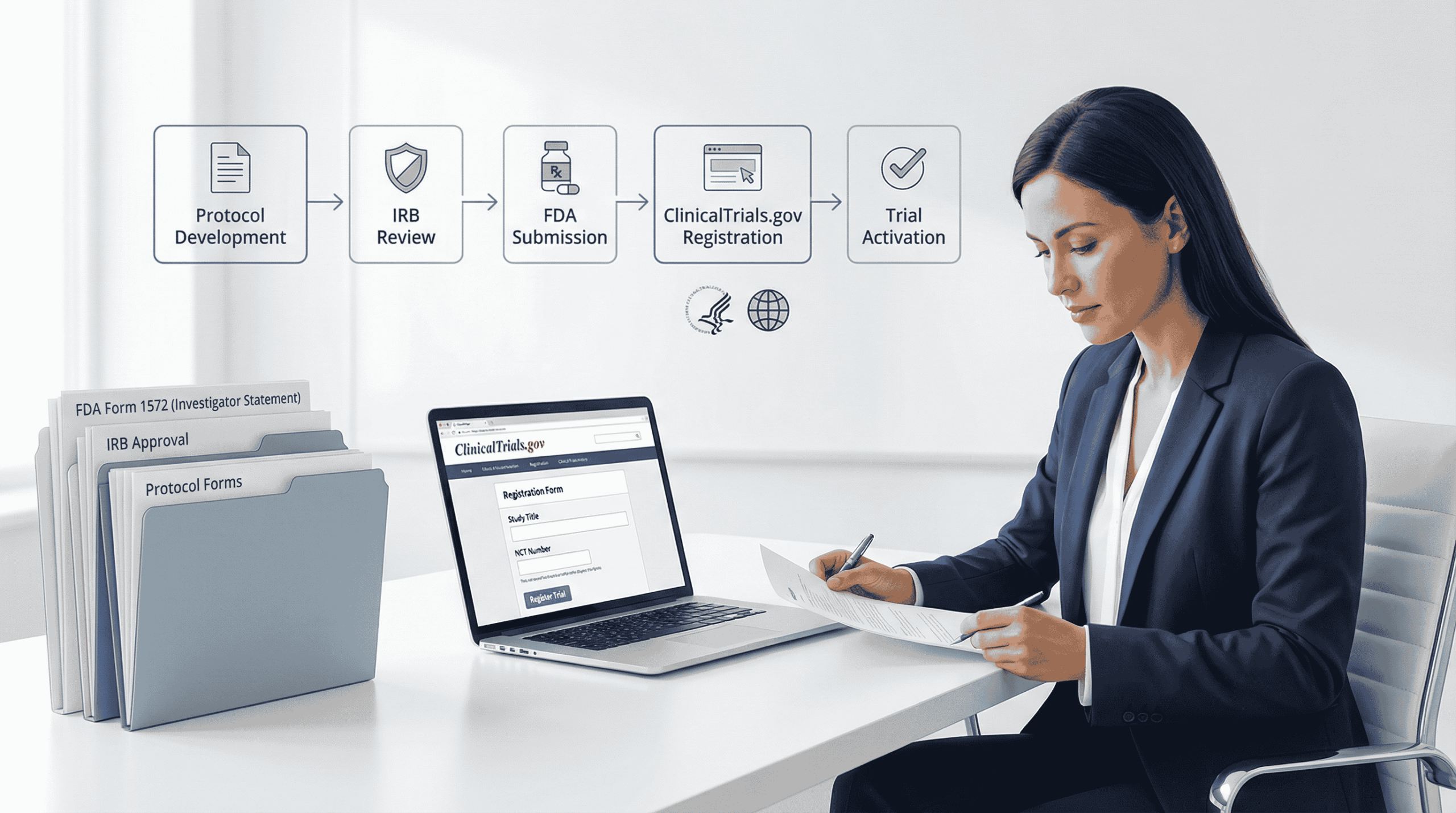
According to educational guidance from the National Institutes of Health, clinical trials follow structured processes designed to protect participants and ensure informed decision-making.
Step-by-Step Overview of Joining a Clinical Trial
The steps in clinical trials are designed to help participants feel informed, protected, and respected throughout the process.
Step 1 – Finding a Trial That May Be Right for You
Most people begin by searching for trials that match their health condition, location, or personal interest. Trials may be found online, through healthcare providers, or through trusted health communities.
You can explore clinical trials by condition and basic eligibility details in one clear place, making it easier to understand available options and next steps: https://decentrialz.com/clinical-trials/condition
first step help you find the right or matching trial for you.
Step 2 – Eligibility Check and Pre-Screening
Once you express interest, you may be asked a few basic questions. These often include age, general health information, current medications, or details about your condition.
Not everyone qualifies for every study, and that is intentional. Eligibility checks protect participants and ensure the study is appropriate and safe for those involved.
If a study is not a match, you are informed clearly and respectfully, and you may be guided toward other opportunities.
Step 3 – Reviewing Study Information and Consent
Before any testing or participation begins, you receive detailed information about the study. This includes what the study involves, how long it may last, possible risks, and your rights as a participant.
This process is called informed consent. You are encouraged to take your time, ask questions, and discuss the information with family or trusted advisors if you wish.
Agreeing to review the information does not mean you are required to participate.
Step 4 – Screening Visits
If you decide to move forward, screening visits may be scheduled. These visits can include health checks, lab tests, questionnaires, or conversations with study staff.
Screening helps confirm whether the study is a good fit for you. It is important to know that screening does not guarantee enrollment, and being screened out is a normal part of clinical research.
Step 5 – Enrollment or Next Steps
If you meet all the study requirements, you may be officially enrolled. The research team will explain what happens next, including visits, follow-ups, and expectations.
If you are not eligible, the decision is shared respectfully, and your time and interest are always valued. Transparency is a key part of joining a clinical trial.
How Long Does It Take to Join a Clinical Trial?
The timeline for joining a clinical trial varies from study to study. Some participants move through the process quickly, while others may experience longer timelines due to additional screening steps or scheduling needs.
Delays often occur to ensure accuracy, safety, and proper review. Understanding this can help reduce anxiety and set realistic expectations.
The time required for joining a clinical trial depends on screening steps, study design, and participant availability.
Understanding the Patient Experience in Clinical Trials
A positive patient experience in clinical trials is built on clear communication and ongoing support. Participants typically receive regular updates, have a clear point of contact, and are informed about what happens at each stage.
Privacy and data protection are taken seriously, and personal information is handled securely. Participants are supported throughout the process, from the first conversation to the final follow-up.
A positive experience while joining a clinical trial depends on communication, respect, and ongoing support.
Common Questions Participants Have Before Joining
Is it safe?
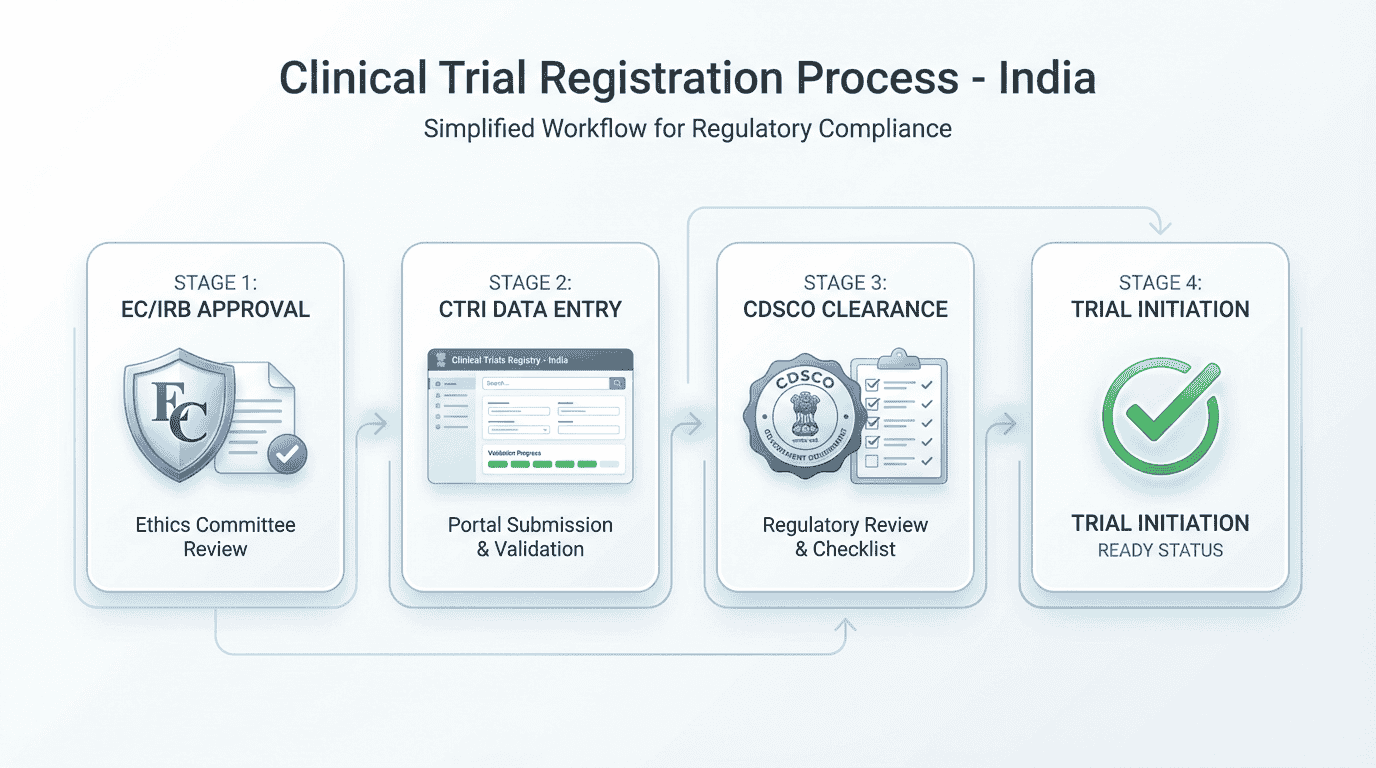
Clinical trials follow strict safety guidelines and are reviewed by ethics committees before they begin.
The U.S. Food and Drug Administration provides clear guidance on participant protections, safety monitoring, and informed consent in clinical trials.
Can I leave the study?
Yes. Participation is voluntary, and you can withdraw at any time.
Will I be paid?
Some studies offer compensation. Details are explained before you decide.
Who do I talk to if I have questions?
You will always have access to a study contact or nurse for support.
How DecenTrialz Supports a Clear and Guided Participant Experience
DecenTrialz is designed to make each step of joining a clinical trial easier to understand and less overwhelming for participants. The focus is on clarity, communication, and respect for individual choice throughout the process.
Only basic information needed for initial pre-screening is collected, helping participants move forward without unnecessary complexity. Registered nurses follow up with participants to clearly explain study requirements in plain language and answer questions before any decisions are made.
Participants are informed about what the next step may be before moving forward, so there are no surprises. When applicable, guidance is provided through the informed consent process to ensure participants understand their options and rights.
Clear status updates are shared during pre-screening and referral, helping participants know where they stand at every stage of the journey.
Learn more about DecenTrialz here:
https://decentrialz.com/about-us
Find a Trial That Fits You
If you are considering participation or simply want to explore options, you can take the next step at your own pace.
Find a Trial That Fits You
https://decentrialz.com/clinical-trials/condition