The future of clinical trial recruitment is shifting away from manual outreach and broad targeting toward more precise, data-driven, and technology-enabled approaches.
As clinical trial protocols become more complex and eligibility criteria more specific, traditional recruitment methods are struggling to keep pace. Sponsors face growing pressure to enroll the right participants faster while maintaining data quality, regulatory compliance, and predictable timelines.
Manual site outreach, general advertising, and referral-heavy strategies often generate high interest but low eligibility yield. This imbalance contributes to screen failures, increased site burden, and delayed enrollment milestones. In response, sponsors are increasingly exploring AI-enabled systems, mobile apps, and digital workflows to improve how participants are identified, assessed, and referred.
Why Recruitment Models Are Changing
Patient recruitment in clinical trials has become one of the most critical operational challenges for sponsors. Enrollment delays remain a leading cause of study extensions, increased costs, and protocol amendments.
Several factors are driving the shift away from traditional recruitment models. Protocols now include narrower inclusion and exclusion criteria, making it harder to identify suitable participants through broad outreach. Screen failure rates continue to rise as sites spend time evaluating participants who do not meet protocol requirements. At the same time, sponsors are expected to deliver more predictable timelines and stronger feasibility assumptions earlier in the study lifecycle.
These pressures have highlighted the limitations of recruitment approaches that prioritize volume over fit. Sponsors are increasingly focused on improving early eligibility alignment and gaining better visibility into recruitment performance before sites become overburdened.
The Role of AI in Clinical Trial Recruitment
AI plays a growing role in future clinical trial recruitment by improving how eligibility criteria are interpreted and applied across large and diverse patient populations.
AI patient matching tools analyze protocol requirements alongside structured and unstructured participant data to identify patterns that suggest eligibility or mismatch. Rather than relying solely on manual prescreening, these systems support earlier identification of participants who are more likely to meet study criteria.
This approach helps reduce protocol mismatch at the top of the recruitment funnel. By improving referral quality earlier, sponsors can lower screen failure rates and reduce unnecessary workload at the site level. AI does not replace clinical judgment but supports it by providing consistent, data-informed insights that improve recruitment efficiency.
Mobile Apps and Digital Touchpoints in Recruitment
Mobile apps have become an important component of digital clinical trial recruitment by expanding reach and improving how potential participants engage with studies.
Through mobile apps, individuals can review study information, respond to eligibility questions, and provide structured data more quickly than through traditional phone or paper-based processes. This improves responsiveness and reduces delays in early-stage recruitment.
For sponsors, mobile apps support more standardized data capture across geographies and sites. Structured inputs make it easier to assess referral quality and reduce variability introduced by manual workflows. When integrated into broader recruitment systems, mobile apps contribute to more efficient and participant-friendly enrollment processes.
Data-Driven Targeting and Early Funnel Visibility
Clinical trial digital patient recruitment emphasizes the importance of visibility early in the recruitment funnel. Sponsors increasingly need insight into how participants move through initial eligibility steps and where drop-offs occur.
Data-driven targeting allows sponsors to monitor referral quality before sites activate fully. Early visibility helps identify whether outreach strategies are producing participants who align with protocol requirements or generating avoidable screen failures.
By understanding recruitment performance earlier, sponsors can adjust targeting strategies, refine eligibility logic, and allocate resources more effectively. This reduces reliance on reactive problem-solving later in the study and supports more predictable enrollment planning.
Reducing Screen Failures Through Better Matching
Screen failures represent a significant operational cost for both sponsors and sites. Poor early alignment between protocol criteria and participant profiles leads to wasted effort, longer timelines, and increased administrative burden.
Future clinical trial recruitment models focus on early eligibility alignment to reduce these inefficiencies. Using structured criteria mapping and instant match logic, recruitment systems can compare participant information against protocol requirements before site involvement.
This improves the quality of referrals sent to sites. Rather than managing high volumes of unsuitable candidates, site teams can focus on participants who are more likely to enroll. For sponsors, this translates into improved timelines, better site relationships, and more reliable enrollment metrics.
Operational Benefits for Sponsors
Technology-enabled recruitment provides several operational advantages for sponsors. Earlier prescreening supports faster enrollment readiness and reduces the administrative load placed on sites. Improved referral quality leads to more efficient use of site resources and fewer delays caused by repeated screening failures.
Data-driven recruitment also supports better forecasting and planning. With clearer visibility into recruitment performance, sponsors can make more informed decisions about timelines, site activation strategies, and risk mitigation. These benefits are especially important for complex or competitive studies where enrollment uncertainty can significantly impact development programs.
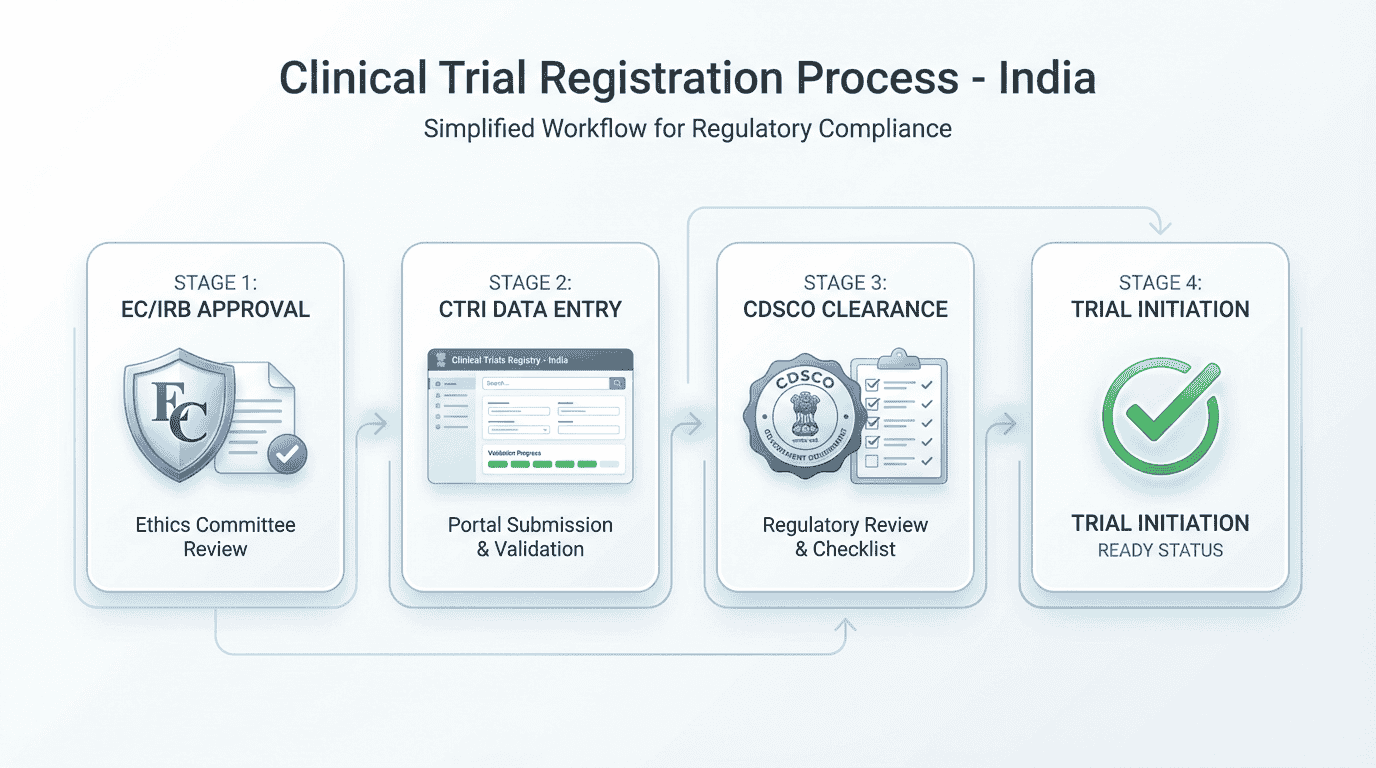
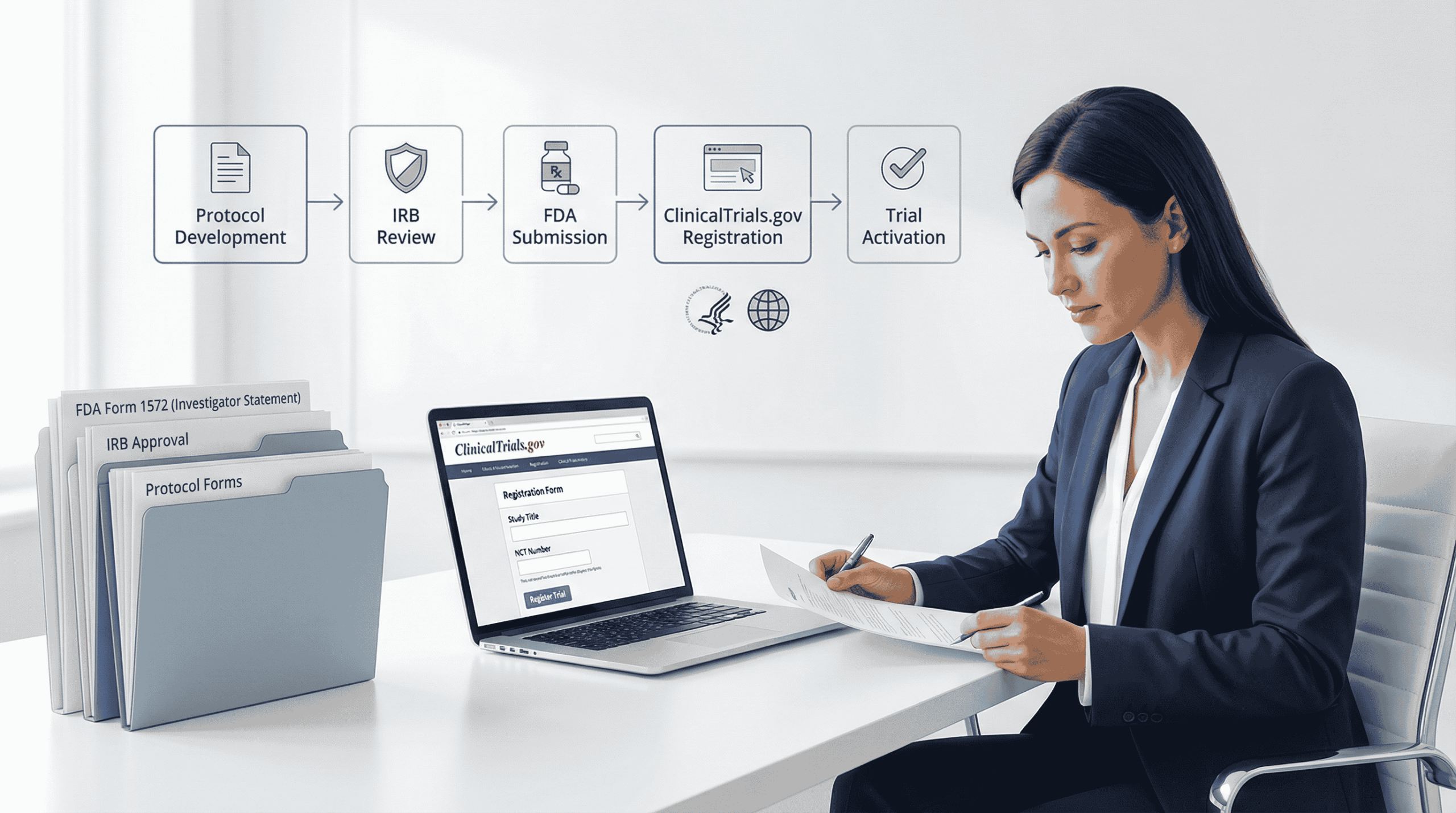
Regulatory and Compliance Considerations
As digital recruitment tools become more widely adopted, regulatory and compliance considerations remain central to sponsor decision-making. Recruitment technologies must support secure handling of personal and health data, transparency in eligibility logic, and auditability across the recruitment process.
Guidance from organizations such as the U.S. Food and Drug Administration emphasizes that digital tools used in clinical research should uphold participant protections while enabling innovation. Responsible use of AI includes clear documentation, appropriate human oversight, and adherence to data privacy expectations.
Sponsors adopting digital recruitment approaches should ensure that systems are designed with compliance, accountability, and ethical use in mind.
How DecenTrialz Is Approaching Smarter Recruitment
DecenTrialz approaches future clinical trial recruitment by applying structured, compliant approaches to eligibility alignment, prescreening workflows, and early-stage referral assessment. This approach is designed to reduce inefficiencies before site activation and provide sponsors with clearer visibility into recruitment performance. Sponsors interested in learning more can visit the DecenTrialz sponsors page, explore data-informed perspectives on the DecenTrialz blog, or learn more about the company’s background and principles on the About Us page